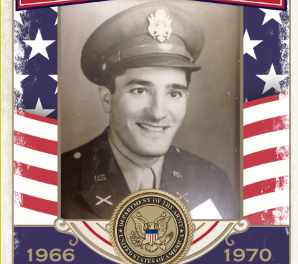
John Mihalcin giddy ups in this photo from his birthday in October. Mihalcin died May 4 after battling COVID-19-contributed photo.
Danielle Toro said she tries not to drive herself crazy when she thinks about the last two-and-a-half weeks of her father’s life. As a Christian, she believes God has a plan, and she has faith in it.
Yet, there are a lot of “what ifs” in the story of John Mihalcin, who died May 4 following a battle with COVID-19 — especially because her mother, Linda, also got sick, and survived.
Mihalcin, 76, of Brookfield, started noticing symptoms April 20, and he was tested that day, the result coming back later as positive for COVID-19. He wasn’t eating or drinking, and he had fallen a couple of times, said his son, Dr. Derek Mihalcin, a licensed psychologist.
On April 22, the Mihalcins’ 53rd wedding anniversary, Mihalcin was taken to the hospital.
Even so, the family never really had an understanding as to how sick he was, Toro said. Linda Mihalcin had been in touch with the health department while he was still at home, and they had said he was doing great and that she should keep him at home.
When the family decided Mihalcin needed to go to the hospital, the ambulance crew wasn’t convinced he was sick enough, Toro said.
At the hospital, the medical care staff said they were considering sending Mihalcin to a rehabilitation center, she said.
“I think we kept getting these messages of hope,” Toro said. “Even when he was in the hospital, he was on three blood pressure medications, to two, to one, to nothing. We just kept getting, like, ‘He’s moving in the right direction.’”
Mihalcin was overweight, diabetic and had a colostomy bag, but he was active. The family was planning a vacation to the beach and, just before getting sick, he had golfed with two grandsons. Toro said the family wanted him to get all the care that was available because he had been so active and involved in the lives of his children and grandchildren. That included pushing for Mihalcin to receive a donation of blood plasma from someone who had recovered from COVID-19 – known as convalescent plasma – and had lined up a donor, someone who already had a letter from the American Red Cross saying she was eligible to donate.
The U.S. Food and Drug Administration has started a clinical trial on an emergency basis to determine if antibodies from recovered virus patients are an effective treatment for sick virus patients, and Mihalcin’s doctors put in a trial treatment for him. He was put on a waiting list.
“We weren’t sure if it was going to be, like, the ‘Hail Mary,’ but it was our hope” that he would receive the plasma, Toro said.
However, the Red Cross cut off allowing donors to designate who received their donation. The family protested, even starting a petition drive.
“At this time, the Red Cross is not asking patient families and physicians to proactively identify donors as this process often delays the product further while requiring additional resources to meet an individual need,” said Regina E. Boothe Bratton, the Red Cross external communications manager for biomedical field marketing and communications for the Greater Chesapeake Bay and Greater Allegheny Regions.

John and Linda Mihalcin-contributed photo
“It is critical we devote our resources and efforts to collecting and building a larger supply of readily available convalescent plasma to meet the broader demand for all patients in need,” Boothe Bratton said. “This also allows the Red Cross to ensure patients receive products in accordance with a fair and equitable process.”
“Each day, we are making strides to get more donors in the door and more products to patients,” said Christy Peters, who shares Boothe Bratton’s title, but serves the Northwest Ohio Region. “While this waiting period continues to decrease, we recognize that it is longer than anyone wants, particularly patients and their loved ones, and we are doing everything we can to reduce that waiting period by focusing our resources and efforts on building that critically needed supply. The Red Cross is grateful to recovered COVID-19 patients who have stepped up in an effort to help someone in need during this difficult time.”
Toro said she was in touch with a Philadelphia woman who had received convalescent plasma from a family member through the Red Cross. She said her doctor had fought for her to receive the plasma, so the Mihalcin family pressed John Mihalcin’s doctors to do the same.
On May 3, the family was told that UPMC had supplied convalescent plasma for Mihalcin, and that he would receive it the next day.
At about 6:30 the next morning, Dr. Mihalcin was in touch with his dad’s doctors, who said his father had had a good night. However, in mid-afternoon, Dr. Mihalcin got word from the doctors that his father was faltering. He had not been given plasma, because the hospital had to wait for the FDA to approve the treatment. The approval had come in about 30 minutes before the call, but the plasma had to be thawed before it could be administered.

The Mihalcin family-contributed photo.
“My brother, I heard him say, ‘Why didn’t you have the plasma ready?’” said Toro, who was part of the Face Time discussion with Dr. Mihalcin and John Mihalcin’s doctors. “This is a desperate family just trying to help him. They said that you can’t thaw the plasma until they get the call. It’s not legal. In case something happened and they couldn’t use the plasma, it wouldn’t be any good.”
Mihalcin died later that day.
Mrs. Mihalcin was not part of the discussion concerning his funeral arrangements because she had become very sick.
“She couldn’t even lift her head up,” Toro said.
Still, the family knew more about COVID-19, and Toro said she believes that made a difference in her mother’s recovery.
“We had a plan where we were gonna take her and what we were gonna do and what we were looking for,” Toro said.
Mrs. Mihalcin’s doctor prescribed measures such as steroids and inhalers to support her lung health, and she turned the corner quickly after beginning the medication. She never had to go to the hospital.
“My mom, she’s doing good,” Toro said on May 26. “She’s started back at work. She gets really winded and she’s tired, but she’s out, she’s moving around.”
Colt Mihalcin, John and Linda’s grandson, lived with them, and he also tested positive for COVID-19. He also is back to work, although he gets winded and had not got his senses of smell or taste back.
Looking back on her father’s treatment, Toro said communication between the family and the medical care staff should have been better.
 “I don’t know where the miscommunication lies,” she said. “I feel like there could have been a better plan of action tailored to him. When you have somebody with those kinds of problems, I think maybe they should have been taken more seriously and maybe a more serious plan of action instead of just, ‘Oh, he’s doing great. Let’s send him to rehab.’ We really thought he was OK. I guess it’s new for everybody, but I think we would have gotten into action more or jumped ahead with some things with him had we known, instead of have that kind of false belief.”
“I don’t know where the miscommunication lies,” she said. “I feel like there could have been a better plan of action tailored to him. When you have somebody with those kinds of problems, I think maybe they should have been taken more seriously and maybe a more serious plan of action instead of just, ‘Oh, he’s doing great. Let’s send him to rehab.’ We really thought he was OK. I guess it’s new for everybody, but I think we would have gotten into action more or jumped ahead with some things with him had we known, instead of have that kind of false belief.”