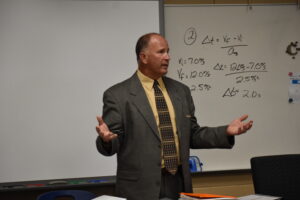
Joe Zuhosky
Editor’s note: This story is part of a series on the 2022 inductees into the Brookfield Distinguished Alumni Hall of Fame.
Dr. Joe Zuhosky’s medical specialty, physical medicine rehabilitation, got its start during the Civil War, when many soldiers suffered amputated limbs.
“That’s when they started devising prosthetics, orthotics and those things,” said Zuhosky, a 1985 Brookfield High graduate.
The specialty moved onto patients with spinal cord injuries, traumatic brain injuries, “anything that would cause someone to lose function or have disability,” he said.
Zuhosky said he sees a lot of patients with back pain – which is the number three cause of disability in the world – neck pain and sports injuries.
At the time that Zuhosky came out of his medical training, patients needing his care often would see him after a surgeon had declined to operate, or an operation had failed.
“I said, ‘This isn’t right,’” Zuhosky said. “Why should the nonsurgical person be the last person you see, and we’re just making everyone go to surgery?”
 Putting the physical medicine rehabilitation doctor at the front of a patient’s medical care puts additional burdens on the doctor, burdens Zuhosky embraced.
Putting the physical medicine rehabilitation doctor at the front of a patient’s medical care puts additional burdens on the doctor, burdens Zuhosky embraced.
“If you’re gonna be at the front of care, you gotta be really good at musculoskeletal medicine and diagnostics,” Zuhosky said. “You better know how to read MRIs; you better know how to read CT scans. You better understand physical therapy principles. You have to have some advanced skill techniques, being able to do interventional procedures, so you’re not just limited to medications and therapy. You better be able to diagnose when they’ve got a true nerve condition. My specialty does all those things.”
Then, if the patient still has issues, surgeons get a look, he said.
“You had to have confidence to stand toe to toe with neurosurgeons and orthopedic surgeons and say, ‘They should see me first, because I’m better equipped to handle this and, if I can’t get them better, then certainly we’re gonna send them to you, if they need surgery,’” Zuhosky said.
“It seems like a really simple concept, and now it is, but you have to convince the surgeons. The surgeons I work with, they love the model, because they know that by the time they’re gonna see the patient we’ve already tried everything that should be done, short of surgery. If it didn’t work, they need surgery.”
Zuhosky, who works at Carolina Neurosurgery and Spine, Charlotte, N.C., said that approach is being adopted by more and more practices.
“The last 25 years of practicing it’s been a huge paradigm shift, and I was really on the very front edge,” he said. “It’s been very gratifying.”
The graduate of Notre Dame University and the Ohio State University College of Medicine came to medicine after being a very young patient who spent a lot of time in the hospital for transfusions – he had a rare internal bleeding condition, Meckel’s diverticulum disorder – surgeries and procedures.
“Some of the medical care was really good, and I really appreciated how nice the nurses were,” Zuhosky said. “In all honesty, some of it wasn’t. Some of the people were really mean to me, even as a kid, and I was terrified. A couple times, I thought for sure I was gonna die.”
“I think having a series of experiences like that as a kid kind of made me want to go into medicine, and help people have a different and better experience.”
Zuhosky served residencies at Northwestern University and the Rehabilitation Institute of Chicago.








